Indo-Hopkins Partnership Seeks Causes of Sepsis in the NICU
Sepsis among newborns in the neonatal intensive care unit (NICU) is a big problem in India, and a complex one to untangle. Infection is typically caused by Klebsiella, E. coli, Acinetobacter, Pseudomonas, and Staphylococcus, and the culprits can be challenging to identify. However, even more confounding is the story of how newborns acquire infection in the first place. Hopkins neonatologist Dr. Julia Johnson notes, “We know that India bears a disproportionate share of disease globally, and we want to know what leads to sepsis—is underlying degree of illness a factor, is infection transmitted from an infected mother, are suboptimal infection control practices to blame? Identifying major causes will help prioritize future development of intervention strategies that will have greatest impact.”
Rate of Sepsis among Neonates in India Not Well Defined
There are a number of ways to define sepsis, and reporting practices in India vary widely, so the actual rate of hospital acquired infection among neonates in India is difficult to pin down. As Dr. Johnson pointed out, “retrospective studies we’ve reviewed suggest it lies somewhere between 6.5 and 38 infections per 1000 live births, depending on how it’s defined.”
That’s a really wide spectrum. But stacking up even the lowest estimate against the US rate of 0.3 infections per 1000 live births provides insight into the scale of the problem. And factoring in differences in population and birth rate between the two countries, the numbers become particularly grim to consider.
In a CDC-funded effort led by Dr. Yuka Manabe, Dr. Johnson is heading a team of Johns Hopkins researchers and NICU experts across 4 Pune, India, medical institutions to describe the root causes of neonatal sepsis. The study—Healthcare-Associated Sepsis in the Neonatal Intensive Care Unit in Pune, India—began in February 2017, and will continue for a year. This study is serving as the basis for an interventional study slated for early 2018 that will focus optimizing infection control practices related to hand hygiene and central line insertion and maintenance, among other practices.
Partnering institutions are located in Pune, India. Dr. Johnson explained why the study is so geographically contained: “Risk factors for sepsis and epidemiology are very country specific, and they even vary regionally within countries. By confining the study to one locale, we hope to be able to figure out why it happens in Pune.” The study is being conducted at Byramjee Jeejeebhoy Government Medical College (BJGMC) and Sassoon General Hospitals; Dr. DY Patil Medical College, Hospital, and Research Centre; King Edward Memorial Hospital (KEM); and Bharati Vidyapeeth Medical College and Hospital (BVDU). All institutions are providing daily patient-level data for analysis.
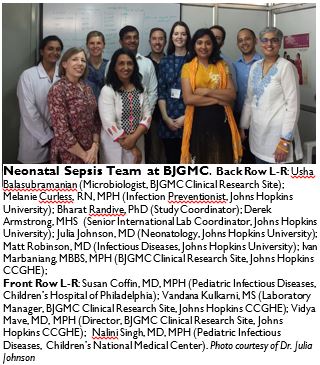
Dr. Johnson and other researchers traveled to the sites in February 2017 to kick off the study. The Hopkins–BJGMC clinical research partnership, led by Drs. Amita Gupta and Vidya Mave, was the first to begin enrolling participants. The study duration is one year, and will include all inborn and community born infants. Johnson expects that more than 3000 newborns will be followed.
When asked what she suspects the team will find, Johnson said “I suspect there are a variety of causes of neonatal sepsis, many of which we will be able to address with infection control process interventions that will be locally feasible and cost-effective to implement.” She added, “Ultimately we want this work to be able inform the development of interventions that help practitioners in Pune save infants from preventable deadly infection. We hope this will lead to interventions that can be scaled up in India and other resource limited settings.”
